When brain cells
fire rhythmically and in sync, they produce waves, which are categorized by
their firing frequencies. Delta waves (1.5 Hz to 4 Hz), for example, are
produced during deep sleep, theta waves (4 Hz to 12 Hz) occur during running
and deep meditation, and gamma waves (25 Hz to 100 Hz) are associated with
excitement and concentration. Disruption of gamma waves could be a key contributor
to Alzheimer’s disease pathology, according to a mouse study published December
7, 2016 in Nature. And the restoration of these waves, researchers propose, may
one day be an option for Alzheimer’s disease treatment.
When a crowd starts to applaud, each person initially
does so to their own rhythm. But in some cases, those claps can synchronize,
with hundreds or thousands or millions of hands striking in unison.
Something similar happens in the brain. When a single
neuron fires, it sends an electrical pulse down its length. But large networks
of neurons can also fire together, creating regular cycles of electrical
activity that resemble the synchronized applause of a rapturous crowd.
Formally, these are called neural oscillations; more colloquially, they’re
brain waves.
These waves are classified by how frequently the neurons
fire in a single second. If they fire one to four times, that’s a delta wave,
which occurs during deep sleep. If they fire 12 to 30 times, that’s a beta
wave, which is typical of normal wakefulness. And if they do so 30 to 90 times,
that’s a gamma wave, which has been linked to higher mental abilities, like
memory, attention, and perception. It’s no surprise, then, that scientists have
seen disrupted gamma waves in many types of brain disorders, including
injuries, schizophrenia, and Alzheimer’s disease.
But by studying mice, Hannah Iaccarino and Annabelle
Singer have shown that these disrupted gamma waves aren’t just a symptom of
Alzheimer’s. By restoring normal gamma waves, Iaccarino and Singer actually
managed to counteract a hallmark of the disease. In Alzheimer’s, a protein
called beta-amyloid gathers in the spaces between neurons, and creates large,
harmful plaques. But gamma can apparently mobilize the immune system to clear
these plaques.
This is still preliminary work, but it heralds a
completely new approach to dealing with Alzheimer’s—changing neural activity,
rather than delivering drugs or chemicals. “It’s so different from what people
have tried, but we are very excited about the possibility of bringing this to
human testing,” says Li-Huei Tsai, an MIT researcher who led the study.
“It’s potentially transformative,” and not because of its
medical implications, says Vikaas Sohal, from the University of California, San
Francisco, who was not involved in the study. “Many neuroscientists, including
myself, have traditionally thought about gamma oscillations as having a role in
how neurons communicate and process information. We haven't really thought
about how they could change the biology of cells. Put it another way: If gamma
oscillations are part of the software of the brain, this study suggests that
running the software can alter the hardware.”
Indeed, that software sometimes gets ignored. According
to Tsai, scientists have made huge progress in understanding the genes and
molecules that underlie Alzheimer’s. But there’s been relatively less work on
how the disease affects the collective activity of neurons—or vice versa.
Her team began by letting mice run through a maze, and
recording the brain waves in their hippocampus—a part of the brain that’s
involved in navigation and memory. Typically, when the mice hit a dead end,
you’d see a short, sharp burst of gamma waves. But when the team studied a
breed of rodents that are especially prone to Alzheimer’s, they saw weaker
gamma bursts, and less synchronicity between the firing neurons.
Earlier studies had found gamma disruptions in people and
rodents with Alzheimer’s. But with one recent exception, these had always
looked at individuals who were already in the late stages of the disease. By
contrast, Tsai’s rodents had no large beta-amyloid plaques, and were totally
asymptomatic. They were early in their disease, and yet they already had gamma
problems. So what would happen, Tsai wondered, if they fixed those problems?
To find out, her team used a technique called
optogenetics, in which neurons are loaded with light-sensitive proteins so that
they can be activated by flashes of light. By sending 40 such flashes a second,
the team could create gamma waves in the brains of their mice. And after doing
so for an hour, they found that they had roughly halved the levels of
beta-amyloid. “We were very, very surprised,” says Tsai.
The team showed that they had mobilized a class of
janitorial cells called microglia. These patrol the brain, cleaning up dead
cells and harmful proteins. After the gamma burst, the microglia doubled in
both number and size, and started swallowing any beta-amyloid that was lying
around.
It’s likely that gamma waves have other benefits beyond
clearing beta-amyloid. For example, Jorge Palop, from the Gladstone Institute of
Neurological Disease, has shown that enhancing these waves can improve the
memories of mice with Alzheimer’s. And Sohal has found that the waves can lead
to “profound and long-lasting improvements in learning.”
That’s all encouraging, but it’s only useful to human
patients if we can induce gamma waves on demand. Optogenetics probably isn’t
the solution: It’s a complicated and invasive technique that is only starting
to find its way into human trials. Fortunately, Tsai’s team have developed a
much simpler procedure.
By simply exposing mice to lights that had been
programmed to flicker at a specific frequency—no protein loading involved—they
managed to induce gamma waves, excite the microglia, and reduce beta-amyloid
levels. They even managed to clear beta-amyloid plaques in older mice that were
further along in their disease.
Using this device, the researchers found that an hour of
exposure to light flickering at 40 hertz enhanced gamma oscillations and
reduced beta amyloid levels by half in the visual cortex of mice in the very
early stages of Alzheimer’s. However, the proteins returned to their original
levels within 24 hours.
The researchers then investigated whether a longer course
of treatment could reduce amyloid plaques in mice with more advanced
accumulation of amyloid plaques. After treating the mice for an hour a day for
seven days, the rodent’s plaque counts fell by two-thirds, as did the size of
the remaining plaques. “That is the most exciting part of this entire study,”
says Tsai.
The researchers also performed studies to try to figure
out how gamma oscillations exert their effects. They found that after gamma
stimulation, the process for beta amyloid generation is less active. Gamma
oscillations also improved the brain’s ability to clear out beta amyloid
proteins, which is normally the job of immune cells known as microglia.
“They take up toxic materials and cell debris, clean up
the environment, and keep neurons healthy,” Tsai says.
In Alzheimer’s patients, microglia cells become very
inflammatory and secrete toxic chemicals that make other brain cells more sick.
However, when gamma oscillations were boosted in mice, their microglia
underwent morphological changes and became more active in clearing away the
beta amyloid proteins.
“The bottom line is, enhancing gamma oscillations in the
brain can do at least two things to reduced amyloid load. One is to reduce beta
amyloid production from neurons. And second is to enhance the clearance of
amyloids by microglia,” Tsai says.
There are still many unanswered questions, though. It's
still unclear why gamma waves are disrupted in Alzheimer’s, or how these waves
excite the microglia. And so far, her flickering lights can only induce the
waves in the visual cortex—a part of the brain that receives signals from the
eyes, and that’s relatively unaffected by Alzheimer’s. The team will need to
find ways of stimulating gamma waves in deeper parts of the brain.
And they’re trying. Together with Ed Boyden, one of the
creators of optogenetics and a contributor to the new study, Tsai has founded a
company called Cognito Therapeutics to develop devices for visually inducing
gamma waves— “googles, or something similar,” she says.
Tsai noted that if it can be developed into a treatment,
light therapy has the advantage of not needing to bypass the blood-brain
barrier, as drugs do. As a non-pharmaceutical treatment, it is likely to have
significantly fewer side effects.
Most significantly, Tsai emphasized that the treatment
relies on the body’s own immune system, rather than an external agent.
“We just directly recruit other neurons and other cell
types in the brain to sort of enable the brain’s inner ability to repair
itself,” Tsai said.
In the meantime, she urges caution. “I worry that people will think they can use a homemade device to treat
themselves, and the correct frequency is extremely important,” she says. “If people use an incorrect one, we don’t
know if it could be harmful. For human use, we need to do more work.”
The further studies are underway, and the preliminary
results are really encouraging. Should you need to wait for the proper model
validation, you try anything right away. There is definitely a strong
precaution, posted above, that using incorrect frequency can be harmful. But if
you sure that the frequency is correct, should you still try? Well, as
scientists say, more than 90% of all trial models, tested positively on mice,
proved to be non-repeatable or n on-sustainable on humans, so if you are a
careful person, stop here, and wait for protocol development. But if you are on
early stages of disease, and you wish to try anything to slow down or reverse
it, go ahead and try it.
The suggested protocol should start with 5 minutes a day,
and to be extended to 1 hour a day in case on no observed side effects and
substantial improvement in your cognitive activities with obvious reversal of
the Alzheimer’ symptoms. Stop immediately if you feel dizzy or unwell,
experience uncharacteristic hallucinations or headaches. Proceed to the full
regime with extreme caution.
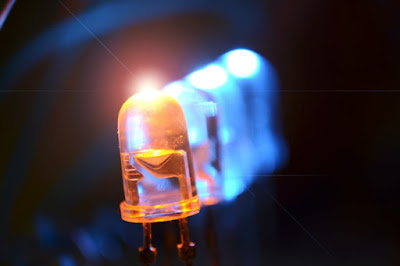
The following video can be used for your light therapy
exercises.
Enlarge the video to a full screen, put a timer for the
desired interval, relax and look on the screen. Stop in any, even minor,
warning call to your current wellbeing.
Sources and
Additional Information:
http://www.naturalnews.com/2016-12-16-light-as-medicine-flashing-lights-found-to-halt-alzheimers-disease.html